Recurrent Abortion Definition:
Occurrence of 3 successive losses (spontaneous abortions) of clinically recognized pregnancies before 20 wk.
– In our practice, we start investigating after 2 failed clinical pregnancies.
– Ectopic & molar pregnancies are not included.
Recurrent Abortion History:
o If there was uterine instrumentation? To rule out adhesions.
o If the menstrual cycle is normal? To rule out endocrine dysfunction.
o If there is premenstrual spotting? To rule out LPD.
o If there is menorrhagia? To rule out fibroid.
o If there is hypomenorrhia? To rule out hypoplastic uterus &Asherman $.
o If there is galactorrhea? To rule out hyperprolactinemia.
o If there is a history of congenital abnormalities or karyotypic abnormalities, which may be heritable?
o If fetal cardiac activity ever detected? RPL before detection of cardiac activity suggests
a chromosomal abnormality.
o If there is consanguinity? To rule out genetic disorders.
o If there is exposure to environmental toxins, which may be lethal to developing embryos?
o If there is a history of venous or arterial thrombosis suggestive of AP$?
o What information is available from previous laboratory, pathology & imaging studies?
o What is the timing? 1st▲ is usually dt. CFMF, while 2nd▲ is usually dt.local cause.
o What is the order? Ascending in uterine hypoplasia & descending in incompetent cx.
o Character of abortus? Fresh in local cause, macerated in maternal disease & malformed in CFMF.
Recurrent Abortion Examination:
– With attention to signs of endocrinopathy (e.g. hirsutism, galactorrhea).
Uterine assessment:
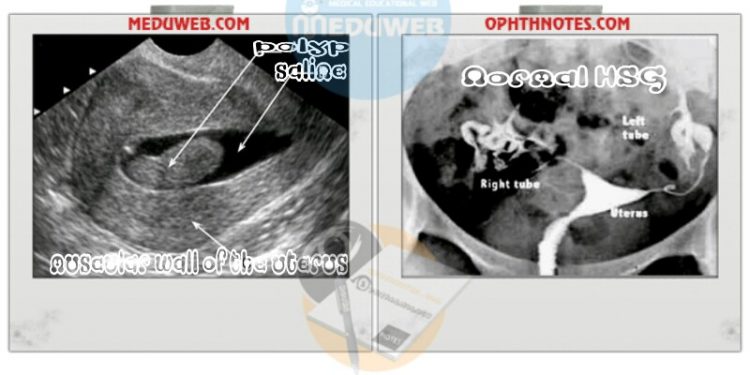
Anatomic causes of RPL are typically diagnosed using HSG or sonohysterography.
•••Sonohysterography:
– More accurate than HSG & gives more information than U/S alone about uterine abnormalities.
– It delineates the internal contours of the uterine cavity & provides concomitant sonographic visualization of the outer surface & wall of the uterus.
– See image down.
•••Hysterosalpingogram (HSG):
– It provides more information about tubal anatomy & patency.
– See images down.
•••Hysteroscopy:
– Hysteroscopy is considered the standard for diagnosis & treatment of intrauterine abnormalities.
•••U/S:
– Useful for the diagnosis of a septate uterus & provide information about the presence and location of uterine myomas.
– Transvaginal U/S (TVS) also provides information about the possibility of cervical insufficiency during pregnancy.
•••MRI:
– MRI is useful for distinguishing between a septate&bicornuate uterus suspected on U/S or HSG.
Anticardiolipin Ab and lupus anticoagulant:
– The minimum immunology work-up for women with RPL is measurement of anticardiolipinAb (IgG&IgM) & lupus anticoagulant.
– Both tests should be done twice, 6-8 wk apart, because a low to mid positive level can be due to viral illness then revert to normal.
– The anticardiolipinAb titer is considered elevated if medium or high titers of both IgG&IgM are present in blood.
Thyroid function tests and thyroid peroxidase antibodies:
– Should be done for women with clinical manifestations or with history of thyroid disease.
– Screening asymptomatic women for subclinical thyroid dysfunction can be offered as there is evidence of an increased risk of abortion in women with subclinical hypothyroidism & in euthyroid women with thyroid peroxidase Ab.
Karyotyping of couples and abortus:
– This is the last test we obtain & only if the above examinations are normal.
– It is part of the evaluation of RPL, despite the low yield of abnormality, cost & limited prognostic value.
– The purpose is to detect balanced translocations that could be passed to the fetus unbalanced.
– Chromosomal abnormalities detectable in parental peripheral blood preparations are an indirect & limited indicator of fetal karyotype. So, many experts also recommend karyotype of the abortus or products of conception.
Screening for DM should be limited to women with clinical manifestations.
Screening for inherited thrombophilia.

Recurrent Abortion Management according To the cause
Uterine abnormalities:
– If uterine septum, intrauterine adhesions or submucosalmyoma, hysteroscopicmetroplasty can be done.
– Repair of bicornuate & septate uteri reduce the abortion rate from 85% (before surgery) to 10% (after surgery).
– Prophylactic cervical cerclage in women with no history of cervical insufficiency isn’t advised.
Antiphospholipid $: Aspirin & heparin improve the pregnancy outcome.
Women with overt thyroid disease or DM should be treated.
Polycystic ovary (PCO): Metformin can be used to decrease the risk of abortion (which is 20-40%), but the effectiveness is NOT proved.
Hyperprolactinemia: Treatment with bromocriptine even in the absence of overt hypogonadism.
Parental karyotype abnormality:
– Parental karyotyping may be indicated in couples with ≥3 clinical miscarriages.
– In <10% of couples, one partner (mostly the mother) will be diagnosed with a balanced translocation. So, we can test the mother first followed by the father as needed.
– Couples in whom chromosomal abnormalities are discovered in one or both partners or the abortus are generally referred for genetic counseling.
– They should be informed about the probability of having a chromosomally normal or abnormal conception in the future.
– IVF with preimplantation genetic diagnosis (PGD) can be used to avoid transfer & implantation of an affected embryo.
– PGD improves the pregnancy outcome of translocation carriers with a history of repeated pregnancy loss.
– For evaluation of products of conception (POC): gestational tissue can be cultured on placenta or blood & kept in normal saline & NOT formalin.
Treatment options for unexplained RPL (40%):
1. Stop smoking, alcohol, caffeine & reduction in BMI (for obese women).
2. Progesterone: We typically prescribe progesterone (200 mg 3 times/day, vaginally) as empiric treatment of unexplained RPL. It is started 3 days after the LH surge, so as not to inhibit ovulation & continued until 10 wk of pregnancy (when placental progesterone production is sufficient).
3. Human menopausal Gn (hMG): Ovarian stimulation via hMG is effective for treatment of endometrial defects in women with RPL. The mechanism may be correction of a luteal phase defect or stimulation of a thicker endometrium, so leading to a better implantation site.
4. IVF &preimplantation genetic diagnosis.
Unproven therapies:
– Aspirin with or without heparin.
– Low-molecular weight heparin (LMWH).
– Human chorionic gonadotropin (HCG)