Anesthetics in Ophthalmic practice
✍ reversible blockage of nerve fiber conduction (block sodium channels) Anesthetics in Ophthalmic Practice
✍ PH dependent for Anesthetics in Ophthalmic Practice:
(less effective at low pH like inflamed tissue)
Classes ( esters and amides)
✍ Ester for Anesthetics in Ophthalmic Practice:
hydrolyzed by plasma cholinesterase
metabolized in liver
Examples
cocaine
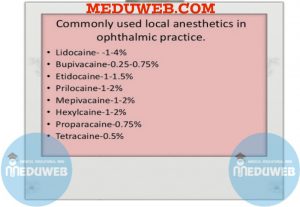
tetracaine (amethocaine)
proparacaine
procaine
benoxinate
✍ Amide Anesthetics in Ophthalmic Practice:
longer duration and less systemic toxicity
metabolized in liver
Examples
lidocaine
mepivacaine
bupivacaine
Routes of administration
✍ Topical Anesthetics in Ophthalmic Practice:
Disturb intercellular junction of corneal epithelium (increase permeability)
Examples
Proparacaine (Ophthaine)
• 10- to 30-minute duration
• cause allergic dermatitis
Tetracaine (Pontocaine)
•similar to proparacaine but longer duration
• more toxic to corneal epithelium
Benoxinate
• similar to proparacaine
• can be combined with fluorescein (Fluress) for tonometry
Cocaine
• greatest epithelial toxicity
• excellent anesthesia
• sympathomimetic effect (test for Horner’s syndrome)
✍ Parenteral( injectables) for Anesthetics in Ophthalmic Practice:
May be used with epinephrine (1:100,000) to increase duration by preventing systemic absorption and decreases bleeding
Hyaluronidase (Wydase) 150 IU increases tissue penetration, but decreases duration.
Side effect of retrobulbar anesthesia 1⁄4 respiratory depression, bradycardia
Toxicity: hypotension, convulsions, nausea, vomiting
Examples
Lidocaine (Xylocaine)
• 1 hour duration (2 hours with epinephrine)
• used for local anesthesia and akinesia
Procaine (Novocain)
• 30 to 45 minute duration
Mepivacaine (Carbocaine)
• 2 hours duration
Bupivacaine (Marcaine)
• 6 hours duration
✍ General Anesthetics in Ophthalmic Practice:
All agents decrease intraocular pressure (IOP)except ketamine, chloral hydrate, N2O, and ether
Malignant hyperthermia (Major complication)
✍ Rare anesthetics in Ophthalmic Practice
✍ autosomal dominant
✍ Occurs after exposure to inhalation agents (most commonly halothane, also succinylcholine, haloperidol
✍More common in children and males
✍ Due to calcium-binding disorder with increased intracellular calcium, which stimulates muscle contraction and interference with oxidative phosphorylation causes hypermetabolic crisis
✍Most have defect in ryanidine receptor (RYR-1 gene on chromosome 19q13.1)


